The Hidden Efficiency Crisis Lab Managers Overlook: Why Equipment Investments Aren’t Translating to Real Capacity Gains
You’ve invested in new diagnostic equipment. Your team learned the procedures. Supplies are stocked. Yet somehow, your laboratory’s efficiency hasn’t improved proportionally to your capital investment. In fact, your costs continue climbing, your staff seems more overwhelmed than before, and you’re still sending samples out to reference labs for results that take days to return.
This isn’t a coincidence. This is the fundamental flaw built into traditional hematology analysis workflows that labs across the healthcare system have accepted as inevitable.
The Real Problem: You’re Paying for Speed Without Getting Velocity
Traditional hematology analyzers deliver a paradox that the industry rarely discusses openly. They complete CBC counts in 2-3 minutes using impedance technology—cells passing through a sensor, generating quick electrical signals translated into numbers. On paper, this looks like speed.
But here’s what actually happens in your lab:
Results arrive fast, but they’re incomplete. Results flagged as abnormal require immediate manual microscopic review—the exact manual process your automation was supposed to eliminate. Your technician stops everything to examine cells under the microscope, adding 15-45 minutes per abnormal sample. In labs where 15-30% of samples require manual review, this “fast” analyzer actually creates a bottleneck that negates every efficiency gain.
The math becomes brutal: a 2-minute result followed by 30 minutes of manual microscopy isn’t speed. It’s an illusion masking a workflow that demands more expertise, constant vigilance, and manual intervention. You’ve automated the easy part while retaining all the labor-intensive complexity that drains your budget and wears out your staff.
Three Hidden Costs Nobody Mentions When Selling You Equipment
The Labor Cost That Never Went Away
Healthcare faces a cataclysmic staffing crisis. The average clinical laboratory worker is aging, replacements aren’t materializing, and turnover rates exceed 25% annually in many markets. Hospitals report finding specialized hematology technicians nearly impossible to recruit.
Traditional analyzers don’t solve this—they mask it. Yes, they automate basic counting. But all the complexity moves downstream: manual microscopic reviews, quality control oversight, flagged result investigation, and regulatory documentation. You’ve shifted work, not eliminated it.
Labs implementing older analyzer technology report that staff spend 40-50% of their time on manual microscopy reviews and quality verification—the exact tasks that supposedly “automated” equipment was supposed to handle. This creates a hidden crisis: you can’t process more samples without hiring more skilled labor you can’t find. Your equipment capacity increases, but your actual throughput remains constrained by staff you don’t have and can’t recruit.
The result? Your $200,000+ investment in equipment creates the need for additional staffing expenses that completely offset any efficiency gains.
The Supply Chain Vulnerability That Worsens With Every Equipment Addition
This crisis has a name: complexity multiplication. Each piece of equipment you add requires separate calibration procedures and reagent management, specialized maintenance and service contracts, consumable supply chains and cold storage requirements, staff training on device-specific protocols, LIS integration and troubleshooting, and quality control documentation and monitoring.
When supplies are scarce—and they frequently are, as we learned during disruptions—fragmented equipment ecosystems become vulnerability multipliers. One disrupted reagent supply means one instrument down. You’ve replaced single points of failure with multiple points of failure. Your diagnostic capacity becomes hostage to supplier reliability across multiple vendors.
Labs maintaining 4-5 separate diagnostic instruments face a mathematical reality: they experience equipment downtime 4-5 times as frequently as facilities with consolidated systems. When uptime matters—when patient care depends on diagnostic results—this fragmentation directly impacts clinical outcomes.
The Capacity Paradox: More Equipment, Lower Throughput-Per-Dollar
Here’s the equation nobody highlights in equipment proposals: Capital investment increases. Per-test costs remain high or increase. Total cost of ownership climbs. Yet throughput gains plateau.
Why? Because traditional workflows hide inefficiency in manual steps that no amount of equipment automation can eliminate. You need the microscope. You need the skilled technician. You need the quality assurance protocols. You need the maintenance technician. None of these disappear with faster counting equipment.
The real economic breakthrough comes not from incrementally faster counting, but from eliminating the manual microscopy review process entirely. That’s the bottleneck destroying your capacity gains. That’s where your budget actually goes.
The Industry Shift Nobody Anticipated: AI-Powered Cell Morphology Changes the Equation
For decades, hematology analysis relied on two core methodologies: microscopy (1850s technology)—manual, slow, highly operator-dependent, extraordinarily expensive in labor—and impedance counting (1970s technology)—fast counting, limited information, requires manual morphological verification.
In 2017, a new paradigm emerged: AI-powered cell morphology analysis. This combines advanced optical imaging capturing cell structure and characteristics at high resolution (4-megapixel imaging), deep learning algorithms trained on 40+ million real clinical samples, automated image analysis identifying cell abnormalities without human intervention, and complete diagnostic reports in 6 minutes—including comprehensive morphological assessment.
This isn’t an incremental improvement. This is a fundamental redefinition of what “automated hematology” actually means.
Here’s the difference:
| Factor | Traditional Impedance | AI-Powered Morphology |
| Result speed | 2-3 minutes | 6 minutos |
| Morphological assessment | Manual microscopy required | Automated, included |
| Manual review rates | 15-30% of samples | <5% of samples |
| Effective turnaround | 30-60 minutes | 6-10 minutos |
| Labor requirements | High (microscopy + QC) | Low (mostly monitoring) |
| Technician expertise needed | Advanced pathologist-level | Basic operator training |
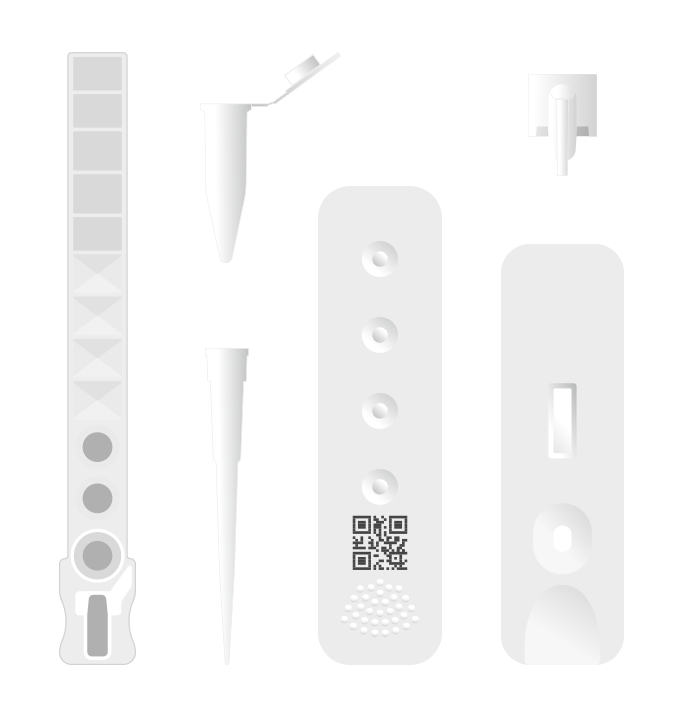
| Supply chain complexity | Multiple reagent systems | Single-use cartridges, room temp |
| Maintenance burden | Significant (calibration, cleaning) | Maintenance-free |
The implications are staggering. Instead of pretending to automate while hiding complexity in manual processes, AI morphology analysis actually delivers what “automation” was supposed to mean: real capacity gain with lower labor requirements.
New Industry Demands Reshaping Laboratory Economics
Three major trends are forcing this conversation:
Decentralized Diagnostics Is No Longer Optional—It’s Mandatory
Healthcare systems increasingly recognize that centralizing all diagnostics in hospital labs is economically unsustainable. Point-of-care testing that delivers lab-grade results in minutes at the patient site represents the future of healthcare delivery.
This means primary care clinics, urgent care centers, rural health facilities, and pharmacies need diagnostic capability previously available only to hospitals. But they can’t maintain complex equipment, can’t employ specialized technicians, and can’t justify $50,000+ capital investments for basic CBC testing.
This demand shift forces the industry question: Can we deliver laboratory-grade diagnostics in a system so simple that non-laboratory staff can operate it reliably?
Traditional equipment cannot answer this question affirmatively. AI-powered systems can.
Labor Market Dysfunction Is Permanent
The laboratory staffing crisis isn’t cyclical—it’s structural. Healthcare employers compete with other industries for workers. Younger generations don’t enter clinical laboratory technology at historical rates. Geographic maldistribution means rural areas have essentially zero access to qualified technicians.
Hospitals can no longer assume they’ll staff their labs with experienced microscopists who can rapidly identify abnormal morphology and make nuanced clinical calls. Instead, they must build workflows where capable equipment compensates for staff limitations.
Equipment that requires expert technicians—traditional impedance systems where manual microscopy review is mandatory—becomes increasingly untenable. Equipment that operates reliably with minimal expertise becomes strategically essential.
Regulatory and Reimbursement Pressure on Lab Economics
Reimbursement bodies are squeezing laboratory economics. Clinical laboratory payment schedules reduced payments for many tests 15-40% over the past decade. Simultaneously, quality and accuracy standards have risen dramatically.
This creates an impossible equation for labs using older technology: maintain quality and accuracy while absorbing lower reimbursement and higher labor costs.
The only mathematical solution is equipment that genuinely reduces per-test costs through elimination of manual labor steps, maintenance-free operation (no service calls), efficient reagent use (lower consumable costs), reduced staff training requirements, and faster turnaround enabling capacity gains.
Traditional equipment can’t deliver this solution. Newer technology can.
Measuring the Real Cost of Traditional Systems: A Scenario-Based Analysis
Consider a 200-bed hospital’s diagnostic lab processing approximately 150-200 hematology tests daily.
With Traditional Impedance Analyzer:
- Equipment cost: $150,000
- Annual consumables: $35,000
- Maintenance and service: $12,000
- Staffing (2.5 FTE at $55,000 salary): $137,500
- Quality control oversight (0.5 FTE): $27,500
- Manual microscopy reviews (estimated 25% of samples): $8,500
- Downtime and errors: $5,000
Total annual cost: $225,500 Cost per test: $3.75/test Capacity: Limited by manual review workload; often cannot process all samples same-day
With AI-Powered Morphology System:
- Equipment cost: $185,000 (higher initial investment)
- Annual consumables: $22,000 (efficient cartridges)
- Maintenance: $0 (maintenance-free design)
- Staffing (1.5 FTE at $55,000 salary): $82,500 (reduced requirement)
- Quality control oversight: Automated (essentially $0)
- Manual microscopy reviews: Minimal ($500)
- Downtime: $0 (no complex maintenance failures)
Total annual cost: $107,000 Cost per test: $1.78/test Capacity: 300+ tests daily possible; can handle 100%+ volume increase without additional staff
Five-year comparison:
| Metric | Traditional | AI-Powered | Advantage |
| Total 5-year cost | $1,252,500 | $648,000 | $604,500 savings |
| Cost per test (5-year avg) | $3.28 | $1.70 | 48% reduction |
| Lab capacity (tests/day) | 150-200 | 300-400 | 100%+ growth |
| Staff required | 3 FTE | 2 FTE | 1 position freed |
| Service calls/downtime | 8-12 annually | 0 | Eliminated |
The breakthrough isn’t faster counting. It’s total cost elimination through genuine automation.
What Changes When Labs Make This Transition
Labs that implement AI-powered hematology analyzers consistently report:
Operational improvements: Turnaround times drop from 60+ minutes to 6-10 minutes, manual review rates fall from 20-30% to <5%, reference lab send-outs for morphological assessment decrease 80%+, same-day results become standard, and capacity increases 50-100% without additional staff.
Financial improvements: Per-test costs drop 35-50%, labor costs decline 25-35% through reduced microscopy workload, maintenance costs approach zero, reference lab savings reach $5,000-15,000 annually, and ROI timeline shortens to 18-36 months.
Clinical improvements: Earlier detection of hematologic abnormalities, reduced missed diagnoses from manual review fatigue, faster treatment initiation for critical patients, better outcomes in sepsis and other acute conditions (where each hour of diagnostic delay increases mortality), and improved triage accuracy through rapid comprehensive assessment.
Staff improvements: Technicians transition from routine counting/microscopy to complex case analysis, manual microscopy work decreases dramatically, staff satisfaction improves (less repetitive work), training burden decreases (simpler workflows), and career advancement paths emerge (focus on complex diagnostics).
The Real Question Facing Lab Managers Today
Your current hematology analyzer delivered what the industry promised: fast counting. But it didn’t deliver what you actually needed: genuine capacity expansion with lower labor and cost.
Traditional equipment reached its technological limit decades ago. Speed improvements now come through added complexity—multiplex testing, advanced flagging, increased parameters—all of which require more expert interpretation.
The breakthrough happens elsewhere: in systems where advanced technology replaces human expertise rather than just assisting it. Where AI morphology analysis eliminates manual microscopy review. Where room-temperature, single-use cartridges eliminate complex supply chains. Where maintenance-free design eliminates service dependencies.
This isn’t about buying more equipment. It’s about fundamentally restructuring your diagnostic workflow to actually deliver automation—not pretend automation.
The labs that make this shift don’t just process more samples. They transform their economics, their staff satisfaction, and ultimately their clinical outcomes.
The question isn’t whether you’ll make this transition. The question is when—and whether your facility will lead the shift or follow it.