Understanding Modern Blood Analyzers: What You Need to Know
Blood analyzers have evolved dramatically over the past two decades, transforming from manual microscopy systems to fully automated intelligent diagnostic instruments. Today’s blood analyzers represent the intersection of artificial intelligence, optical engineering, and clinical expertise, offering unprecedented accuracy and efficiency in hematological testing.
When searching for a blood analyzer for sale, it’s essential to understand that modern systems go far beyond simple cell counting. Advanced hematology analyzers now incorporate AI-powered Complete Blood Morphology (CBM) analysis, which identifies not just the quantity but the morphological characteristics and abnormalities of blood cells with pathologist-level precision. This technological advancement has made quality diagnostics accessible to hospitals, clinics, laboratories, and even point-of-care settings worldwide.
The global demand for reliable blood analyzers continues to grow. Healthcare facilities recognize that investing in modern diagnostic equipment directly impacts patient outcomes, operational efficiency, and cost management. Whether you’re operating a high-volume hospital laboratory, a community clinic, or a mobile diagnostic unit, the right blood analyzer can become a cornerstone of your diagnostic capability.
The Evolution of Blood Cell Analysis Technology
The history of blood cell counting spans nearly two centuries. The earliest methods relied on manual microscopy—a labor-intensive approach introduced in the 1850s that required skilled technicians and offered limited standardization. The 1950s brought impedance methods, which used electrical pulses to count cells based on size, dramatically increasing throughput but lacking morphological detail.
The 1970s introduced flow cytometry, a significant advancement that allowed cells to pass through a laser-focused stream for more sophisticated analysis. However, each generation had trade-offs between speed, accuracy, and cost. Today’s AI-powered systems, developed since 2017, combine the morphological insight of microscopy with the speed of automated systems while adding intelligent analysis that rivals expert pathologists.
Modern blood analyzers now incorporate patent-protected technology that has been trained on millions of clinical samples. This deep learning approach enables systems to recognize not just normal blood cells but also identify subtle abnormalities that might indicate disease states ranging from infection to anemia to hematologic malignancies.
Key Features to Look for When Purchasing a Blood Analyzer
When evaluating blood analyzers for sale, several critical specifications determine clinical value and operational success:
Complete Blood Morphology Analysis (CBM) represents the most significant advancement in hematology. Traditional Complete Blood Count (CBC) systems identify only basic white blood cell categories—neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Advanced CBM systems go further by identifying intermediate cell types including immature neutrophils (NST), mature segmented neutrophils (NSG), hypersegmented neutrophils (NSH), abnormal lymphocytes (ALY), platelets with abnormal granules (PAg), and reticulocytes (RET). This expanded analysis provides clinicians with deeper insights into bone marrow function and systemic health.
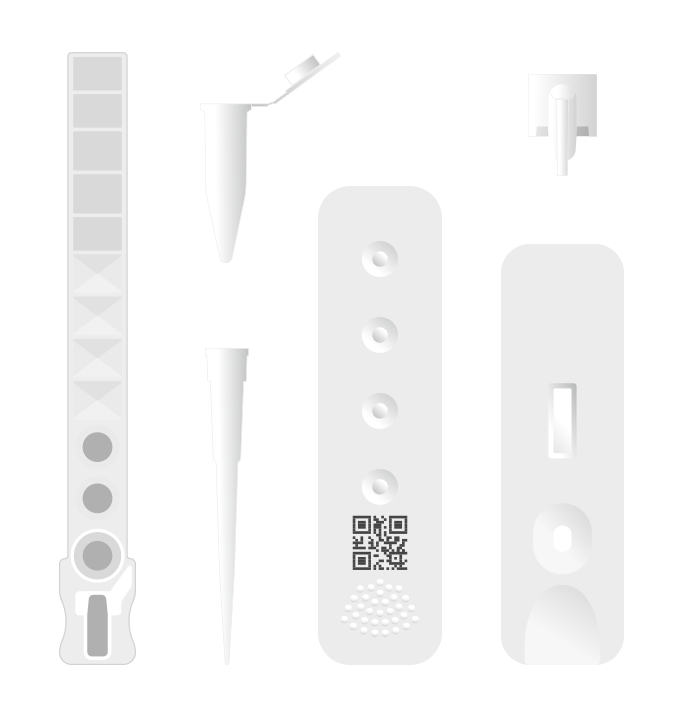
Maintenance Requirements significantly impact total cost of ownership. Modern analyzers using single-use cartridge technology eliminate the need for daily maintenance, system cleaning, and the costly downtime associated with equipment servicing. This design also prevents cross-contamination between samples and eliminates blockage issues common in systems with permanent pipette networks.
Sample Volume Requirements matter for patient comfort and practicality. Advanced analyzers designed for point-of-care use require only 30 microliters of capillary blood from a fingerstick—minimally invasive and particularly valuable when testing children, elderly patients, or patients with compromised venous access. This capability expands the range of settings where professional-grade diagnostics become feasible.
Throughput and Turnaround Time determine operational capacity. Modern systems capable of processing 10 samples per hour with results delivered in 6 minutes enable rapid triage, faster clinical decision-making, and improved patient satisfaction. For emergency departments and acute care settings, this speed directly impacts patient outcomes.
Multi-Functional Capabilities streamline laboratory operations. The most versatile analyzers available today combine hematology, immunoassay, biochemistry, and urine/fecal analysis in a single platform. This integration reduces equipment footprint, simplifies staff training, and enables comprehensive testing from a single sample.
Current Market Applications and Clinical Settings
Blood analyzers for sale serve diverse clinical environments, each with unique requirements:
Hospital Central Laboratories benefit from high-throughput systems processing hundreds of samples daily. Modern analyzers deliver the comprehensive 7-differential counts that pathologists require for complex case management, while automated reporting systems integrate seamlessly with hospital information systems and laboratory information systems.
Point-of-Care and Clinic Settings require compact, user-friendly systems that don’t demand laboratory infrastructure or specialized technician training. Clinic-grade blood analyzers enable immediate decision-making—a physician can obtain complete hematological results within minutes of patient presentation, dramatically improving diagnostic efficiency.
Emergency and Urgent Care Departments depend on rapid turnaround to guide treatment decisions. Analyzers delivering complete blood work in 6 minutes enable faster triage and clinical decision-making compared to sending samples to central laboratories.
Veterinary Practices now benefit from species-specific analyzers that identify not just routine blood parameters but also veterinary-specific markers. Multi-functional veterinary analyzers that combine hematology with urine and fecal analysis address the full diagnostic needs of companion animal medicine.
Mobile and Telemedicine Units utilize compact, portable analyzers that maintain laboratory-grade accuracy while operating in field settings. The minimal sample volume requirement makes mobile diagnostics practical for rural healthcare, disaster response, and preventive health campaigns.
Pharmacy-Based Diagnostics represent an emerging market in countries permitting pharmaceutical testing (including Brazil, Italy, France, USA, Australia, Ireland, and Kenya). This expansion dramatically increases access to diagnostic services.
Advanced Technology: AI and Optical Innovation
The most sophisticated blood analyzers available today incorporate multiple technological innovations working in concert:
Convolutional Neural Networks (CNNs) trained on 40 million+ clinical samples represent the “expert brain” of modern analyzers. These AI algorithms have been formally recognized at international conferences for their ability to identify cell morphology patterns with unprecedented accuracy. Unlike traditional rule-based software, neural networks continuously improve their classification accuracy as they encounter new cell morphologies, effectively “learning” from experience.
Swiss Optical Customized Lens Systems with 4-megapixel resolution and 50 frames-per-second acquisition capture cellular detail approaching oil-immersion microscopy. The optical path includes patented Z-stack technology that captures three-dimensional cell images, providing morphological information that two-dimensional imaging cannot match.
Fully Automated Mechanical Arms with sub-micrometer positioning accuracy (less than 1 micrometer) ensure consistent, reproducible sample positioning and analysis. This mechanical precision eliminates operator-dependent variation and ensures that results are reproducible across time and across different technicians.
Pure Liquid-Phase Staining Technology based on Wright-Giemsa methodology delivers superior cellular detail compared to automated dry-staining systems. The liquid-based approach ensures optimal stain penetration, allowing algorithms to detect subtle morphological features that indicate pathology.
Multimodal Imaging Integration combines visible light imaging with narrowband multispectral imaging to capture complementary information. Integration of multiple imaging modalities provides redundant diagnostic pathways, improving confidence in results.
Regulatory Quality and Safety Credentials
Blood analyzer equipment must meet stringent regulatory standards ensuring patient safety and result reliability. Leading systems in the market today carry comprehensive certifications:
FDA Registration and CE Marking indicate compliance with US and European regulatory frameworks. FDA registration requires demonstration of safety and effectiveness for intended use. CE marking confirms compliance with European medical device regulations including essential health and safety requirements.
ISO 13485:2016 Certification specifies quality management system requirements for medical device manufacturers. This certification requires documented processes for design, manufacturing, sterilization, testing, and post-market surveillance.
ISO 9001 Certification confirms general quality management system compliance across all operations.
Manufacturers with these certifications maintain rigorous documentation of product development, clinical validation studies, manufacturing quality control, and adverse event reporting. These credentials provide assurance that systems undergo appropriate testing before clinical release and that manufacturing maintains consistent quality.
Investment Considerations and Total Cost of Ownership
When evaluating blood analyzers for sale, acquisition cost represents only one component of total investment. Complete financial analysis includes:
Capital Equipment Cost varies based on functionality. Basic 3-differential hematology analyzers represent lower initial investment but offer limited clinical insight. Advanced 7-differential multi-functional systems command higher capital investment but deliver significantly greater clinical utility.
Reagent and Consumable Costs include test kits, calibration controls, and quality control materials. Systems using single-use cartridges eliminate the chemistry-related consumables (oils, detergents, staining solutions) required by systems with permanent reagent networks.
Maintenance and Service Costs range from minimal for cartridge-based systems to substantial for systems requiring regular service visits. Systems designed for “maintenance-free” operation reduce labor costs and equipment downtime.
Training and Workforce Productivity represent often-overlooked costs. User-friendly systems with intuitive interfaces reduce training time and accelerate proficiency, while system reliability and maintenance-free operation minimize downtime costs.
Space Requirements impact facility costs. Compact analyzers optimized for point-of-care use occupy minimal bench space, an advantage in crowded laboratory or clinic environments.
Sophisticated procurement analyses reveal that lower-cost systems may actually increase total cost of ownership through higher consumable expenses, frequent maintenance, and reduced productivity. Many healthcare facilities have discovered that investing in advanced systems reduces per-test costs despite higher initial capital investment.
Integration with Healthcare Information Systems
Modern analyzers for sale today operate as intelligent nodes within healthcare ecosystems rather than standalone devices. Key integration capabilities include:
Laboratory Information System (LIS) Connectivity enables direct result transmission to medical records systems, eliminating manual data entry and associated transcription errors. Two-way communication allows LIS systems to transmit test orders directly to analyzers.
Hospital Information System (HIS) Integration connects laboratory results to clinical workflows, enabling automatic ordering of reflex tests and clinical alerts when results fall outside normal ranges.
Wireless Communication via WiFi, Bluetooth, and cellular connectivity enables remote operation, remote troubleshooting, and central monitoring of multiple instruments across distributed facilities.
Cloud-Based Analytics and Reporting enable sophisticated analysis of laboratory performance metrics, trending analysis, and quality management across multiple locations.
These integration capabilities transform blood analyzers from isolated diagnostic devices into integrated components of clinical decision support systems.
Choosing the Right Analyzer: Matching Technology to Clinical Needs
The optimal blood analyzer depends on specific organizational needs:
For High-Volume Hospital Laboratories: Multi-functional analyzers combining hematology, biochemistry, and immunoassay maximize efficiency and minimize equipment footprint. High throughput (10+ samples/hour) accommodates peak demand periods.
For Community Clinics and Primary Care: Compact, maintenance-free hematology analyzers with intuitive interfaces enable non-laboratory personnel to obtain immediate results. User-friendly operation reduces training requirements.
For Emergency Medicine: Rapid turnaround (6 minutes) and comprehensive reporting enable faster clinical decisions in time-sensitive situations.
For Veterinary Practice: Species-specific analyzers with urine and fecal analysis capabilities address the full diagnostic spectrum of animal medicine.
For Point-of-Care and Remote Settings: Minimal sample volume requirements, room-temperature test kit storage, and standalone operation enable professional-grade diagnostics in non-laboratory environments.
Conclusion: The Future of Blood Diagnostics
Blood analyzers for sale today represent a fundamental transformation in diagnostic capabilities. The combination of AI-powered analysis trained on massive clinical datasets, advanced optical imaging, fully automated sample processing, and seamless information system integration creates diagnostic systems that are simultaneously more accurate, faster, and easier to use than their predecessors.
As healthcare systems globally continue to decentralize diagnostic capabilities and expand access to point-of-care testing, the importance of selecting reliable, validated analyzer systems becomes increasingly critical. Organizations seeking to improve diagnostic accuracy, reduce testing turnaround times, and optimize laboratory efficiency should carefully evaluate advanced systems that incorporate complete blood morphology analysis and modern quality assurance.
For organizations considering blood analyzer purchases, the most important consideration remains matching technology capability to actual clinical needs while ensuring that selected systems carry appropriate regulatory certifications, demonstrate validated clinical performance, and integrate seamlessly with existing information systems.
Learn more about professional-grade blood analyzers and diagnostic solutions at https://ozellemed.com/en/