Introduction: The Foundation of Modern Diagnostics
The Complete Blood Count (CBC) remains the most frequently ordered laboratory test in clinical practice worldwide. This comprehensive panel measures three fundamental cell populations—red blood cells, white blood cells, and platelets—providing clinicians with critical information for diagnosing infections, anemia, hemostasis disorders, and systemic diseases. Understanding CBC analysis, its parameters, and common pitfalls is essential for both healthcare professionals and informed patients.
The evolution from manual microscopy to AI-powered automated analysis has transformed turnaround times from 30-60 minutes to 6 minutes, enabling time-critical clinical decisions in sepsis, acute hemorrhage, and hematologic emergencies.
Understanding CBC Parameters: The Complete Picture
Red Blood Cell (RBC) Parameters: Oxygen Carrying Capacity
The RBC panel includes seven critical measurements that assess oxygen-carrying capacity and classify anemias. RBC Count (normal: males 4.35–5.65 × 10¹²/L; females 3.92–5.13 × 10¹²/L) quantifies total circulating red blood cells. Hemoglobin (normal: males 13.2–16.6 g/dL; females 11.6–15.0 g/dL) is the oxygen-binding protein within RBCs and represents the hallmark marker of anemia severity. Hematocrit (normal: males 38.3–48.6%; females 35.5–44.9%) expresses the percentage of blood volume occupied by RBCs.
The RBC indices enable precise anemia classification. Mean Corpuscular Volume (MCV) (normal: 80–100 fL) measures average RBC size, classifying anemias as microcytic (<80), normocytic (80–100), or macrocytic (>100). Mean Corpuscular Hemoglobin (MCH) (normal: 27–31 pg) indicates average hemoglobin content per cell. Mean Corpuscular Hemoglobin Concentration (MCHC) (normal: 32–36 g/dL) calculates hemoglobin density and represents one of the most stable parameters. Red Cell Distribution Width (RDW) (normal: 12.0–14.3%) quantifies variation in RBC size and serves as an early anemia indicator.
White Blood Cell (WBC) Parameters: Infection and Immunity
Total WBC Count (normal: 3.5–9.5 × 10⁹/L) forms the foundation of immune assessment. Elevation above this range (leukocytosis) suggests acute infection, inflammation, or leukemic processes, while reduction (leukopenia) indicates bone marrow suppression or overwhelming infection.
The 5-Part WBC Differential identifies specific immune cells. Neutrophils (normal: 1.8–6.3 × 10⁹/L) constitute the body’s primary bacterial defense and elevate rapidly during acute infections. Lymphocytes (normal: 1.0–4.0 × 10⁹/L) orchestrate adaptive immunity and increase during viral infections. Monocytes (normal: 0.2–0.8 × 10⁹/L) function as systemic scavengers. Eosinophils (normal: 0.1–0.4 × 10⁹/L) respond to parasitic infections and allergies. Basophils (normal: 0.02–0.10 × 10⁹/L) participate in allergic responses.
Advanced analyzers now detect immature cells—band neutrophils, metamyelocytes, and blasts—providing enhanced early detection of infection severity and hematologic malignancies.
Platelet Parameters: Hemostasis Assessment
Platelet Count (normal: 150–400 × 10⁹/L) directly assesses bleeding risk. Values below 150,000 increase hemorrhage risk, while elevations above 400,000 may indicate reactive inflammation or myeloproliferative disorders. Mean Platelet Volume (MPV) (normal: 7.6–9.3 fL) indicates platelet size; elevated MPV suggests immature platelet release reflecting bone marrow stress. Plateletcrit (PCT) (normal: 0.1–0.28%) reflects total platelet mass.
How CBC Analysis Works: From Sample to Result
Modern CBC analyzers deliver complete results in six minutes through a standardized process. The sample undergoes precise dilution and staining, followed by passage through optical and impedance detection chambers. Individual cells are counted, sized, and characterized simultaneously. Advanced analyzers employ high-resolution digital imaging to photograph individual cells, with artificial intelligence trained on 40+ million clinical samples identifying morphologic abnormalities—a capability traditional analyzers cannot match.
Daily Quality Control Requirements include analysis of three control levels (normal, abnormal, pathologic) before patient testing begins. This 23-minute calibration window, often overlooked in efficiency calculations, represents actual operating time. Analytical Accuracy demonstrates exceptional performance with correlation coefficients exceeding 0.98 across all parameters: WBC r² = 0.9962; RBC r² = 0.9787; Hemoglobin r² = 0.9867; Platelets r² = 0.9834.
Common Errors in CBC Analysis: Three-Phase Framework

Laboratory errors occur across three distinct phases, with pre-analytical errors accounting for 50–80% of all errors—a proportion emphasizing specimen handling criticality.
Pre-Analytical Errors: The Dominant Source (50–80% of errors)
Specimen Collection Problems represent the most frequent errors. Clotted CBC samples account for 64–80% of pre-analytical rejections, followed by hemolysis (5–10%) and insufficient volume (3–7%). Improper tube selection, inadequate mixing, delayed transport, or incorrect anticoagulant ratios all compromise specimen integrity.
Specimen Quality Issues create specific analytical challenges:
- Hemolysis (RBC rupture from rough handling) falsely elevates potassium and interferes with hemoglobin measurement
- Lipemia (elevated blood triglycerides) causes falsely elevated hemoglobin, MCH, and MCHC through optical interference; centrifugation at 10,000 × g for 10 minutes removes this interference
- Clotted Samples prevent accurate measurement across all parameters
Reported Error Frequency: Current literature documents 0.39–0.73% pre-analytical error rates in major hospital laboratories, with clotting as the predominant cause.
Analytical Errors: Equipment and Interferent Issues (10–20% of errors)
Equipment-Related Problems include calibration drift, reagent degradation, and flow cell obstruction. Daily calibration verification is essential; failure to recalibrate after component replacement produces systematic measurement errors.
Specific Interferents generate clinically significant misinterpretations:
- RBC Agglutinins (cold antibodies): Cause false low RBC and WBC counts; resolve through 37°C incubation
- WBC Clumping: EDTA-dependent antibodies cause unmeasurable or severely depressed WBC counts; detected by analyzer flags and microscopy confirmation
- Platelet Agglutinins (pseudothrombocytopenia): Account for 0.1–1% of CBC rejections; incubation at 37°C typically resolves
- Paraproteinemia (multiple myeloma, Waldenstrom): Falsely elevates hemoglobin, MCH, MCHC; identified through elevated MCHC exceeding biological limits (>37 g/dL)
- Cryoproteins: Generate false elevations in WBC and platelet counts at room temperature; require 37°C incubation or warm diluent
Fibrin Clumps and Small Clots obstruct flow cells or elevate WBC counts falsely; analyzer flags alert operators to perform microscopic verification.
Post-Analytical Errors: Interpretation and Reporting (10–20% of errors)
Result Validation Failures occur when analysts inadequately review analyzer flags, ignore delta checks (comparison to previous results), or fail to perform peripheral blood smears when indicated. Data Entry Errors from manual result transcription exceed automated LIS interface errors by 5–10 fold.
Critical Value Notification failures represent high-consequence errors. Immediate physician notification is required for: WBC <2.0 or >40 × 10⁹/L; Hemoglobin <6.6 or >20 g/dL; Platelets ≤10 or >1000 × 10⁹/L.
Clinical Interpretation: Integrating Numbers Into Diagnosis
Anemia Classification Using RBC Indices
Microcytic Anemia (MCV <80 fL) indicates iron deficiency, thalassemia, or lead poisoning. Low RDW suggests pure iron deficiency; normal RDW suggests thalassemia.
Normocytic Anemia (MCV 80–100 fL) with elevated reticulocyte count indicates hemolysis or acute blood loss; low reticulocyte count suggests bone marrow failure or chronic kidney disease.
Macrocytic Anemia (MCV >100 fL) with hypersegmented neutrophils indicates vitamin B12 or folate deficiency; normal neutrophil morphology suggests alcohol use, liver disease, or hypothyroidism.
Infection Pattern Recognition
Bacterial Infection: Elevated neutrophils with left shift (>5% immature forms) indicates acute bacterial infection. Elevated total WBC combined with elevated procalcitonin and C-reactive protein strengthens diagnosis.
Viral Infection: Relative lymphocytosis (normal WBC, elevated lymphocyte percentage) with atypical lymphocytes characterizes viral illness, particularly infectious mononucleosis.
Sepsis Recognition: Severe leukocytosis (>15,000) or severe leukopenia (<4,000) combined with elevated immature forms and toxic neutrophil appearance constitutes a time-critical clinical threshold requiring immediate intervention.
Quality Assurance Protocols: Maintaining Accuracy
Daily Procedures require running three control levels before patient testing, with documented acceptance/rejection criteria. Calibration Requirements mandate daily or weekly recalibration depending on analyzer type; frequency varies by manufacturer and laboratory protocol.
External Proficiency Testing occurs monthly or quarterly, providing comparison with peer laboratories. Manual Microscopy Correlation is required when analyzer flags abnormalities (15–25% of samples in typical labs); peripheral blood smears confirm morphologic findings and detect artifacts.
Comprehensive Documentation includes QC results, calibration records, error logs, corrective actions, and staff competency assessments. This quality system architecture prevents recurrence of identified problems and demonstrates regulatory compliance to CAP and CLIA inspectors.
Advanced Technology: Modern CBC Capabilities
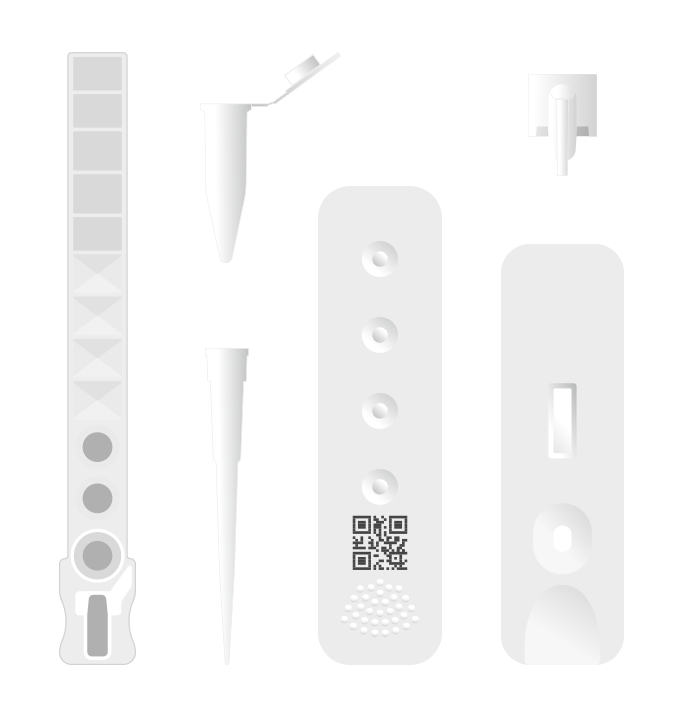
AI-powered Complete Blood Morphology (CBM) analyzers now report 37+ parameters by imaging 10,000+ individual cells per sample—compared to traditional analyzers measuring 20–30 parameters through statistical sampling. This technological advancement enables automated detection of immature cells (blasts, bands, metamyelocytes), morphologic abnormalities (toxic granulations, Auer rods), and left shift, with integrated flags directing technician attention to abnormalities requiring manual verification.
Point-of-Care Testing capabilities allow capillary sampling (40 µL blood) with 6-minute results, enabling rapid decision-making in primary care, emergency departments, and resource-limited settings. Result integration with Electronic Health Records improves clinical workflow efficiency.
Practical Troubleshooting: Solving Real-World Problems
When Results Don’t Match Clinical Presentation, systematically verify: (1) analyzer QC performance and calibration status; (2) delta checks to previous results (significant acute changes warrant repeat testing); (3) flags and alerts generated by analyzer; (4) pre-analytical issues (hemolysis, lipemia, clotting); (5) peripheral blood smear morphology if available.
Common Scenarios:
- Unexpectedly Low Platelets: Check for clumping through 37°C incubation; verify no visible clots in specimen
- High RBC with Low Hemoglobin: Suspect lipemia; perform plasma replacement or high-speed centrifugation
- Unmeasurable WBC: Look for clumping; verify proper mixing; consider redraw if clotting present
Conclusion: Best Practices for Laboratory Excellence
CBC analysis remains foundational to modern clinical diagnostics. Success requires vigilant attention to specimen handling (preventing 80% of laboratory errors), regular quality control and calibration, critical interpretation of analyzer flags, performance of microscopy when indicated, and clinical correlation with patient presentation. Modern automated analyzers with AI-powered morphology provide unprecedented diagnostic capability when integrated with rigorous quality assurance protocols.
For laboratory managers implementing advanced diagnostic capabilities, comprehensive pre-purchase assessment of patient mix, error frequency, throughput requirements, and quality control costs prevents 90% of budget overruns. Ozelle’s AI-powered CBC analyzers represent state-of-the-art technology, available at https://ozellemed.com/en/.