I. Introduction: Why Labs Can’t Afford Fragmented Diagnostics Anymore
Healthcare economics are unforgiving. Hospitals face compressing reimbursement rates, chronic staffing shortages, and escalating equipment maintenance costs. Independent labs and primary care clinics struggle to justify diagnostic investments when reference laboratory send-outs promise “no upfront capital.” Yet this calculus ignores a fundamental truth: fragmented diagnostics cost more—sometimes 40–60% more—when evaluated over their complete lifecycle.
An all-in-one mini-lab represents a paradigm shift. Rather than deploying separate instruments for complete blood count (CBC) analysis, immunoassay testing (inflammation markers, cardiac biomarkers, hormonal assays), and biochemistry (glucose, lipids, organ function), a single consolidated platform handles all three modalities from a unified interface. Ozelle’s EHBT-50 exemplifies this approach: a 7-differential hematology analyzer combined with fluorescence immunoassay and dry-chemistry biochemistry in one compact device.
The strategic thesis is straightforward: consolidated diagnostic platforms reshape lab economics by reducing total cost of ownership (TCO) by 40–60% over five years while simultaneously improving clinical capability, turnaround times, and diagnostic access.
II. The Old Model: Separate Analyzers, Separate Budgets, Compounded Costs
A. Typical Fragmented Lab Setup
Most clinics and small hospitals deploy three to five analyzers independently: a dedicated hematology instrument, a separate chemistry analyzer, an immunoassay platform, and often a urinalysis system. Each operates under its own service contract, requires distinct operator training, and consumes its own supply chain of reagents and calibration materials.
This fragmentation creates hidden operational complexity. Equipment purchase price represents only 20–30% of five-year total cost of ownership; the remaining 70–80% emerges from maintenance, consumables, labor, and infrastructure demands. For a typical three-instrument lab, these compounding costs become substantial.
B. Hidden Costs Beyond Instrument Purchase
Consider the operational burden:
Maintenance and Service: Each analyzer carries an annual service contract averaging $8,000–$15,000, many with per-call overages of $350–$500 when error codes exceed contracted limits. One Midwest clinic documented 47 error events in year one, climbing to 89 events by year two—generating $18,400 in unbudgeted service fees against a $9,600 base contract.
Quality Control Materials: This cost category often surprises budget planners. Most analyzers require dual-level quality control runs every 8 hours, costing $4.80–$7.50 per vial. A clinic operating 16 hours daily needs 6 QC runs per analyzer, 365 days yearly. For three analyzers, this generates $10,000–$15,000 annually—often exceeding 20% of total operating budget by month six, yet buried in purchasing as a minor “accessory” line item.
Reagent Storage Infrastructure: Traditional liquid-phase reagent systems demand refrigeration, water systems for dilution and maintenance, and biological waste processing. These represent indirect costs—utility expenses, environmental compliance, equipment-specific storage spaces—that don’t appear on equipment purchase orders but accumulate over time.
Labor and Staffing: Managing multiple analyzers consumes technologist time. Daily maintenance on three instruments, separate proficiency testing, distinct operator training, and troubleshooting for multiple platforms creates staffing inefficiencies. Error codes on one instrument may require specialized knowledge while another waits idle.
C. Financial Pain Points for Stakeholders
Hospital CFOs: Capital budgets become fragmented across overlapping platforms. A $50,000 CBC analyzer plus a $45,000 biochemistry analyzer plus a $40,000 immunoassay platform equals $135,000 in upfront capital—often with overlapping capability (many measure glucose, perform basic counts, or detect inflammation markers independently). This redundancy represents wasted investment.
Lab Directors: Operational complexity multiplies. Scheduling preventive maintenance on three different platforms, training new technologists on distinct interfaces, and coordinating multiple service vendors creates administrative overhead. Quality control schedules become asynchronous, requiring staff presence at irregular intervals.
Clinic Administrators: The fragmented model makes in-house diagnostics difficult to justify. A clinic processing 200 samples daily might invest $130,000 in equipment plus $25,000 annually in consumables and maintenance. Against reference lab pricing of $8–$15 per test, the financial case becomes marginal unless volumes exceed 2,500–3,000 monthly samples. This threshold excludes many primary care practices from deploying lab capabilities, forcing them into reference lab dependency.
III. What Is an All-in-One Mini-Lab? Technical Overview of the EHBT-50
A. Core Concept: One Platform, Multiple Modalities
An all-in-one mini-lab consolidates three testing modalities into a single automated system: 7-differential CBC with advanced cell morphology analysis, immunoassay capabilities, and dry-chemistry biochemistry testing. The EHBT-50 delivers this integration with 37+ hematology parameters (including advanced markers: NST, NSG, NSH, NLR, PLR, ALY, PAg, RET) plus immunoassays (CRP, SAA, PCT, cardiac troponin, thyroid hormones, sex hormones, inflammation markers) and biochemistry testing (glucose, lipids, renal function, liver function, bone metabolism, HbA1c).
Unlike traditional approaches requiring sample splitting across instruments, the EHBT-50 processes a single venous or capillary draw (30–100 µL) through automated pretreatment, then simultaneously performs CBC imaging, immunoassay detection, and biochemistry colorimetry. A unified touchscreen interface orchestrates the entire workflow.
B. Design Features That Enable Consolidation
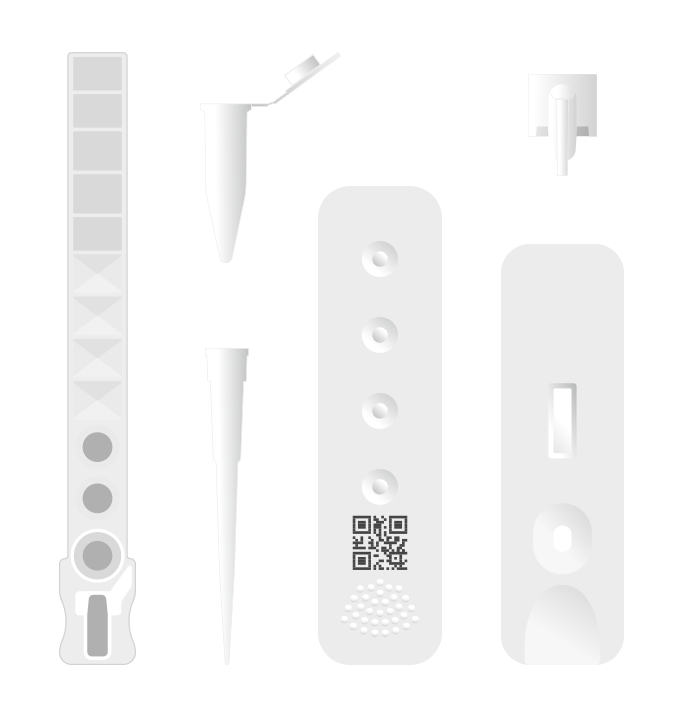
Single-Use Cartridge Architecture: The EHBT-50 employs individual, pre-packaged test cartridges—no pipelines, no liquid reagent storage, no daily flushing cycles. This design eliminates the primary maintenance burden plaguing traditional analyzers. Cartridges are stored at room temperature for two years, eliminating refrigeration infrastructure and reagent deterioration risk.
Maintenance-Free Operation: Without internal plumbing, the instrument requires no daily cleaning protocols, minimal calibration cycles, and no service interventions for clogged lines or reagent carryover. This dramatically reduces hands-on technician time and service contract dependencies.
Unified Workflow: One 10.1-inch touchscreen interface guides operators through sample loading, provides one-click testing, and generates integrated reports in approximately 6 minutes. Staff training requires learning a single interface rather than three separate systems. Throughput reaches 10 samples per hour—suitable for clinic and small lab volumes while supporting high-functioning units.
Connectivity: LIS/HIS integration via WiFi, Ethernet, USB, and Bluetooth ensures seamless data flow. Results populate directly into electronic health records without manual transcription, eliminating a major source of operator error.
C. AI and Complete Blood Morphology (CBM) as the Engine
The EHBT-50’s core innovation is AI-powered CBM technology. Rather than relying solely on impedance pulse counting (which provides only cell size and number), the system combines high-resolution optical imaging with deep-learning classification trained on 40+ million real clinical blood samples.
How it works: Automated staining and high-speed microscopic imaging capture 3D morphological characteristics of individual cells. Convolutional neural networks (CNNs) classify cells with granular precision, identifying not just WBC types (neutrophils, lymphocytes, monocytes) but also abnormal morphologies critical for diagnosis: schistocytes indicating microangiopathic hemolytic anemia, spherocytes suggesting hereditary spherocytosis, immature granulocytes (NST) signaling infection or bone marrow stress.
Clinical advantage: This morphology-based approach reduces manual microscopic review dependency. Abnormal cell flags appear automatically; pathologist oversight becomes confirmatory rather than obligatory. For primary care and clinic labs, this obviates the need for regional reference lab support for blood smear reviews, cutting delays and logistics costs.
AI-Assisted Diagnostic Reports: Beyond simple result reporting, the system provides AI-assisted diagnostic context. When a patient shows elevated CRP plus elevated neutrophil percentage plus immature neutrophil bands, the report flags “possible acute bacterial infection” with reference-range context. This guidance supports clinical decision-making without replacing physician judgment—a critical distinction respecting diagnostic authority while enhancing access to sophisticated analysis.
IV. Where the 40–60% Cost Savings Come From
A. Capital Expenditure (CapEx) Reduction
Replace 3–5 separate analyzers with a single EHBT-50 and the arithmetic is straightforward:
- Traditional setup: CBC analyzer ($60K) + Biochemistry analyzer ($50K) + Immunoassay analyzer ($45K) = $155,000 initial capital
- Consolidated EHBT-50: ~$x’x,000–$x’x,000(For specific pricing, please contact us.)
- Direct CapEx savings: $55,000–$70,000 (35–45% reduction)
Moreover, capital amortization on a single device that covers multiple test modalities generates better return on investment. A single platform serving four test categories improves CapEx efficiency compared to platforms serving narrow menus. This matters for cash-constrained clinics evaluating debt financing or lease arrangements.
B. Operating Expenditure (OpEx) and Total Cost of Ownership
Real savings emerge in operations:
- Maintenance and Service Consolidation
Single service contract (~$8,000/year) replaces three contracts (~$24,000–$30,000/year combined). Error codes occur on one platform, managed through one vendor relationship. No more coordinating multiple on-site visits or managing parallel support escalations.
A five-year comparison: $40,000 (consolidated) vs. $120,000–$150,000 (fragmented) = $80,000–$110,000 saved in service costs alone—offsetting a significant portion of the higher initial EHBT-50 purchase price.
- Quality Control Consolidation
Single QC schedule replaces three. One clinic running the EHBT-50 consolidated their 3×2-level daily QC runs into single coordinated checks covering all three modalities simultaneously.
Calculation:
- Fragmented (3 analyzers): 6 QC runs/day × $6/vial × 2 levels × 365 days = $26,280/year
- Consolidated: 2 QC runs/day × $6/vial × 2 levels × 365 days = $8,760/year
- Five-year savings: $87,600
- Reagent Portfolio Simplification
Fragmented labs maintain 30–50 distinct reagent SKUs across three platforms. Consolidated systems reduce this to 15–20. Inventory management becomes simpler, wastage decreases (fewer expired reagents), and bulk-purchase discounting becomes more achievable.
Studies show 5–10% per-test cost reduction through consolidated reagent procurement, amounting to $2,000–$5,000 annually for a typical clinic.
- Labor and Training Efficiency
Onboarding a technician requires learning one interface instead of three. Initial training time drops from 40–60 hours to 20–25 hours. For a three-person lab adding one technician annually, this represents $1,200–$1,800 in training cost savings.
Ongoing operation also benefits. Daily troubleshooting requires expertise in one system. Scheduled maintenance windows become shorter because only one device requires downtime rather than staggered maintenance on three platforms.
Estimated annual labor savings: $3,000–$5,000 for mid-sized labs; potentially $8,000–$12,000 for larger facilities with dedicated biomedical technicians.
- Space and Infrastructure
The EHBT-50 footprint (350 × 400 × 450 mm, ~15 kg) replaces instruments consuming 8–12 linear feet of bench space. This 60–70% space reduction frees valuable real estate, potentially deferring facility expansion costs or enabling reallocation to higher-value functions (patient areas, phlebotomy stations).
For a hospital planning a new lab build-out, consolidated equipment reduces required square footage, directly lowering construction and HVAC costs. A facility designed around 5 instruments instead of 12 might require 500–800 fewer square feet, potentially saving $50,000–$100,000 in construction expenses.
C. Modeled TCO Scenario: 200-Bed Hospital
Consider a mid-sized hospital processing 500 CBC per day plus routine chemistry and immunoassay testing (150,000 samples annually):
Fragmented Setup:
- Equipment (amortized): $135,000 ÷ 5 years = $27,000/year
- Maintenance & service: $24,000/year
- QC materials: $22,000/year
- Consumables (reagents, controls, waste): $48,000/year
- Labor (dedicated technician): $55,000/year
- Five-year TCO: $298,000
Consolidated EHBT-50 Setup:$x’x,000(For specific pricing, please contact us.)
Savings: 46% TCO reduction
This model excludes avoided reference laboratory send-outs for complex cases (estimated additional $20,000–$40,000 annually for large facilities) and improved revenue from expanded in-house testing capability.
V. Workflow Transformation: From Complex to Streamlined

A. End-to-End Sample Journey
Sample Collection → Loading (30 seconds): Phlebotomist collects 30–100 µL capillary or venous blood into collection tube. Technician loads tube into EHBT-50 sample carousel.
Automated Pretreatment (1–2 minutes): The system automatically performs differential blood cell staining, dilution for CBC counting, and sample preparation for immunoassay and biochemistry modalities—tasks requiring multiple manual steps across fragmented platforms.
Simultaneous Analysis (3–4 minutes): While CBC optical imaging and impedance counting proceed, immunoassay fluorescence detection and biochemistry colorimetry execute in parallel.
Report Generation (6 minutes total): Integrated report displays 37+ hematology parameters, immunoassay results (CRP, SAA, troponin, etc.), biochemistry values (glucose, lipids, renal markers), and AI-assisted diagnostic context—all from a single sample.
B. Clinical Impact on Decision-Making
Consider a patient presenting to the ED with fever and chest pain. Traditional workflow:
- CBC sent to hematology analyzer (10 min wait, result in 15 min)
- Chemistry panel sent to biochemistry instrument (10 min wait, result in 20 min)
- Troponin/CRP sent to immunoassay (5 min wait, result in 30 min)
- Physician waits ~45 minutes for complete assessment
With EHBT-50:
- Single sample load (1 min)
- Resultados completos en 6 minutos
Clinical benefit: 39-minute reduction in diagnostic turnaround. For acute coronary syndrome or sepsis evaluation, this translates directly into earlier intervention—critical interventions where every minute improves outcome probability.
C. Quality and Consistency
AI-powered morphology analysis standardizes CBC interpretation across shifts and technicians. Manual smear reviews introduce inter-observer variability (10–15% disagreement rates documented in literature); CBM algorithms provide reproducible classification.
Unified QC processes replace parallel validation schedules, reducing risk of asynchronous quality lapses where one analyzer underperforms while others remain undetected.
VI. Use Cases Across Different Healthcare Settings
A. Hospital Core Labs and Emergency Departments
Consolidated mini-labs function as satellite platforms complementing high-volume central analyzers. During off-hours or surge periods, the EHBT-50 handles rapid assessment bundles—CBC + CRP + troponin + basic renal function—without queuing to central instruments.
Sepsis Protocol Example: Patient admitted with fever and hypotension. EHBT-50 delivers CBC (identifying left shift via elevated NST), CRP (inflammation marker), PCT (infection severity), and renal function (lactate, creatinine) in 6 minutes. Physician initiates antibiotics based on complete data within 10 minutes of arrival vs. 45–60 minute reference lab delays.
B. Primary Care Clinics and Community Health Centers
This use case transforms clinical economics. A typical primary care clinic screening 100 patients daily can now offer lab-grade CBC, CRP, HbA1c, lipid panel, and renal function in-house—tests previously outsourced to reference labs at $8–$15 per test.
Economic Impact:
- 100 patients × 4 tests/patient = 400 tests/month
- Reference lab cost: 400 × $12 = $4,800/month
- EHBT-50 cost: 400 × $2.50 (consumable) + $666 (amortized equipment/maintenance) = $1,666/month
- Monthly savings: $3,134
- Annual savings: $37,600
Break-even occurs within 2–3 months. Beyond this threshold, every test generates net revenue, improving clinic profitability while enhancing patient experience (same-day results, fewer return visits).
C. Developing Regions and Decentralized Programs
Room-temperature cartridge storage, maintenance-free operation, minimal water requirements, and power efficiency make the EHBT-50 ideal for resource-constrained settings. Indonesia deployment serves 15 clinics across rural areas previously dependent on 2–3 day reference lab turnarounds. Mobile units carrying EHBT-50 systems enable pop-up clinics without requiring permanent laboratory infrastructure.
D. Hybrid Human–Veterinary Platforms
Ozelle’s EHVT-50 extends this model to veterinary medicine, creating synergy for organizations serving both human and animal populations. Integrated diagnostics providers can standardize on platforms supporting both markets, multiplying equipment utilization and amortizing capital across broader service lines.
VII. Strategic Perspective for CFOs and Lab Leadership
A. Building the ROI Business Case
Procurement should demand transparency on lifetime cost:
- CapEx: Equipment purchase or lease terms
- OpEx: Five-year consumable projections based on actual lab volumes
- Maintenance: Service agreements with error-call caps in writing
- Labor: Staffing requirement reduction quantified in hours/week
- Space: Square-footage reduction valued at real estate cost or deferred expansion
One California clinic documented:
- Equipment cost: $85,000
- Five-year consumables: $160,000
- Five-year maintenance: $40,000
- Labor savings (prevented hire): $120,000
- Space avoidance (deferred renovation): $75,000
- Total net benefit: $170,000
The $85,000 equipment investment generated $170,000 in value—a 200% ROI over five years.
B. Risk Management and Scalability
Consolidation reduces vendor complexity. Multi-site networks can standardize on a single platform, enabling bulk service negotiations, unified staff training, and simplified inventory management. One service contract covers 5–10 instruments across departments vs. 15–20 parallel contracts.
Backup strategy matters: organizations should maintain redundancy for critical functions (e.g., two EHBT-50s at a hospital to ensure one failure doesn’t halt diagnostics), but this still costs less than maintaining fragmented backup systems.
C. Future-Proofing Through AI and Over-the-Air Updates
Software updates expand test menus without hardware replacement. Ozelle delivers OTA (over-the-air) updates adding new biomarkers, expanded panels, and AI model improvements. A facility investing in EHBT-50 today gains access to tomorrow’s diagnostic capabilities without capital re-investment.
This aligns with digital health strategies emphasizing cloud integration, predictive analytics, and data-driven decision support—capabilities increasingly central to clinical workflows.
VIII. Implementation Roadmap
Step 1: Baseline Assessment
Inventory current analyzers, service contracts, monthly test volumes, and equipment footprint. Calculate current five-year TCO (often revealing $300,000–$500,000+ for mid-sized labs).
Step 2: Pilot Deployment
Deploy EHBT-50 to one department (ED, primary care clinic, or satellite lab). Track: turnaround time, cost per test, error rates, staff satisfaction, and clinical feedback.
Step 3: Scale and Optimize
Based on pilot outcomes, roll out to additional sites. Standardize protocols, LIS templates, and training curricula across network.
Step 4: Continuous Improvement
Use analyzer-generated data to optimize test bundling, identify high-utilization panels, and predict consumable inventory needs.
IX. Conclusion: The New Normal for Diagnostics
All-in-one mini-lab platforms represent a fundamental shift in diagnostic strategy. By consolidating fragmented systems into unified platforms, labs achieve 40–60% TCO reductions while improving clinical capability, turnaround times, and diagnostic access.
For CFOs facing budget pressures, directors managing operational complexity, and clinic administrators unable to justify in-house testing, consolidated platforms offer compelling economics. Early adopters gain competitive advantage through better margins, superior patient experience, and future-ready infrastructure.
The investment calculus is clear: the question is no longer whether consolidation delivers value, but why any facility would maintain the inefficiency of fragmented diagnostics.
Learn more about all-in-one diagnostic solutions at https://ozellemed.com/en/