Healthcare data breaches cost an average of $7.42 million in 2025, with U.S. breaches averaging $10.22 million—67% higher than the global average. Alarmingly, 1.2 million internet-connected healthcare devices are publicly accessible online, including blood-test systems. Many healthcare organizations report managing IoT devices with known vulnerabilities.
Compact hematology analyzers increasingly integrate with Laboratory Information Systems (LIS), Hospital Information Systems (HIS), and cloud-based telemedicine platforms, creating new attack surfaces for cybercriminals. Healthcare procurement teams struggle to evaluate cybersecurity features when selecting medical devices, while regulatory pressure intensifies through 2025 HIPAA updates, FDA Section 524B guidance, the EU Cyber Resilience Act, and NIS2 Directive compliance.
As compact hematology analyzers evolve into smart, connected diagnostic devices, cybersecurity and data privacy have shifted from optional features to central procurement decision criteria. This article provides hospital IT directors, compliance officers, and procurement leaders with practical frameworks for selecting, deploying, and managing secure connected diagnostic analyzers.
THE CONVERGENCE: WHY COMPACT HEMATOLOGY ANALYZERS ARE NOW CYBERSECURITY TARGETS

The Digital Transformation of Diagnostic Equipment
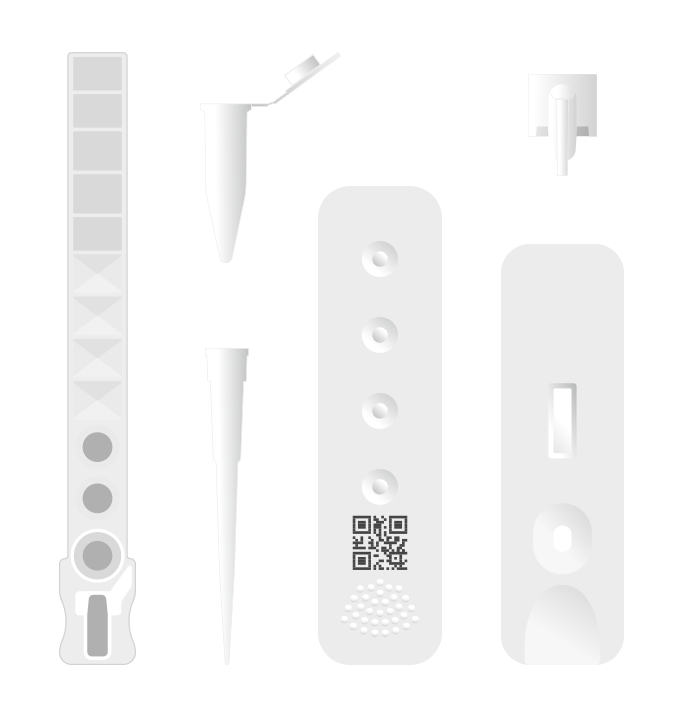
Traditional standalone analyzers have transformed into connected IoT devices transmitting real-time data to EHR/LIS/cloud platforms. Modern compact hematology analyzers offer remote monitoring capabilities, predictive maintenance functionality. Many modern analyzers integrate network capabilities for data transmission and optional cloud-based analytics.
The Expanding Attack Surface
The statistics are sobering: 93% of organizations confirmed KEVs and insecure internet connections for IoT devices. While 75% of healthcare organizations increased IoMT security budgets, only 17% feel confident detecting and containing attacks. One in five connected medical devices runs on unsupported operating systems; merely 13% support endpoint protection agents. Most alarmingly, 21% of medical devices rely on weak or default credentials.
Real-World Consequences
Connected analyzers face multiple threat vectors. Theoretical cybersecurity threats such as data poisoning could compromise system integrity. Ransomware—exemplified by the Ascension Health attack in May 2024—targets diagnostic systems as critical infrastructure. In June 2025, a misconfigured MongoDB database exposed 8 million patient records. Average healthcare breach dwell time: 279 days, providing attackers months to manipulate data.
Patient Safety Directly at Risk
Cybersecurity threats could impact availability or integrity of data flow, which may in turn affect clinical workflows, but actual impact on analytical result accuracy requires specific investigation.
REGULATORY LANDSCAPE: THE COMPLIANCE MANDATE RESHAPING PROCUREMENT

2025 HIPAA Security Rule Updates
HIPAA Security Rule requires covered entities to implement reasonably appropriate access controls (which often include MFA based on risk assessment).
Regular penetration testing and vulnerability assessments are recommended as part of a robust security risk management program per HIPAA guidance. Healthcare organizations bear responsibility for testing devices they procure; vendors must provide penetration testing documentation and vulnerability remediation timelines.
The HHS Office for Civil Rights (OCR) expects full compliance documentation within 10 business days of notice. Failure to document activities can result in escalated penalties. Medical devices are explicitly included in risk assessment scope.
FDA Cybersecurity Guidance (Section 524B)
FDA cybersecurity guidance encourages implementation of SPDF and threat modeling as part of premarket submissions.
International Regulatory Convergence
The EU Cyber Resilience Act imposes mandatory cybersecurity requirements on connected products. NIS2 Directive explicitly targets medical device manufacturers. ISO 81001-5-1 Standard now harmonizes device cybersecurity assessment across Japan, Singapore, and the EU. CE Marking requirements now include AI Act compliance for high-risk AI systems.
Significantly, 73% of healthcare organizations report new FDA and EU regulations already influence device procurement decisions.
THE CYBERSECURITY STACK: TECHNICAL STANDARDS FOR CONNECTED ANALYZERS

Data Integration Standards: HL7 v2 vs. FHIR
HL7 Version 2 represents the legacy standard with segment-based messaging for EHR/LIS/RIS integration. However, it lacks modern security built-in and requires additional encryption and validation layers.
HL7 FHIR represents the modern standard with RESTful API architecture, OAuth2 authentication, encrypted data exchange, and built-in semantic interoperability for AI solutions. Industry trend shows FHIR adoption accelerating for new compact hematology analyzer implementations.
Point-of-Care Device Standards (IEEE 11073)
This standardized communication protocol supports secure device-to-system communication through object-oriented architecture. The Service-Oriented Device Connectivity (SDC) variant enables real-time clinical coordination.
Encryption & Authentication Standards
Transport Layer Security (TLS 1.2+) is mandatory for ePHI transmission per NIST standards. End-to-end encryption protects data at rest and in transit. Role-Based Access Control (RBAC) differentiates user access levels. MFA is now mandatory for remote access under 2025 HIPAA requirements. API Security relies on OAuth2/OpenID Connect for third-party integrations.
PROCUREMENT EVALUATION FRAMEWORK: SELECTING SECURE ANALYZERS
Request for Proposal (RFP) Cybersecurity Requirements
Healthcare organizations should mandate explicit cybersecurity criteria: ISO 81001-5-1 compliance with threat modeling documentation, FDA 510(k) or CE marking including cybersecurity premarket submissions, HIPAA Security Rule compliance assessment, and penetration testing results from qualified third-party assessors.
Secure Software Development Framework documentation should include design controls integrating security from inception, threat modeling identifying attack vectors, security testing protocols, and vulnerability management processes.
Data integration security must specify LIS/HIS integration methodology (HL7 v2 with TLS 1.2+ encryption or modern FHIR/REST APIs), MFA capability for remote access, API documentation detailing authentication and authorization, and third-party integration security protocols.
Vendor Risk Assessment Matrix
Create weighted scoring frameworks assigning percentage weights: Regulatory Compliance (25%), Secure Design (20%), Data Integration (20%), Patch Management (15%), Incident Response (10%), and Operational Support (10%).
Service Level Agreements (SLAs) with Cybersecurity Provisions
Critical SLA components include vulnerability response timelines (30-90 days, risk-based), availability SLA (99.5%+ uptime with explicit security incident exclusions), 24/7 support access, vendor notification within 24-72 hours of breach discovery, cyber liability insurance requirements, and data return/deletion protocols upon contract termination.
DEPLOYMENT & OPERATIONAL SECURITY
Network Architecture & Segmentation
Segregate compact hematology analyzers on isolated network segments, not general hospital WiFi. Implement Zero Trust Architecture verifying every connection. Deploy firewalls and intrusion detection for network monitoring. Use VPN/secure tunnels for remote support access.
Access Control Implementation
Administrative controls include written security policies, designated system administrators with HIPAA training, and regular access reviews. Physical controls restrict access through secure placement and tamper-evident seals. Technical controls mandate changing default credentials, role-based access differentiation, comprehensive audit logging, and session timeouts (15-30 minutes recommended).
Continuous Monitoring & Threat Detection
Track analyzer software versions, patch status, and error rates. Maintain detailed logs of login attempts, failed authentications, and configuration changes. Conduct quarterly vulnerability scans per 2025 HIPAA requirements. Monitor unusual data transmission patterns indicating potential exfiltration.
BUSINESS ASSOCIATE AGREEMENTS & VENDOR ACCOUNTABILITY
If your analyzer vendor accesses PHI, a Business Associate Agreement (BAA) is mandatory. The BAA must explicitly define permitted use, restrict disclosure, mandate HIPAA Security Rule safeguards, address subprocessors, grant audit rights, establish breach notification within 24 hours, and specify data return/destruction protocols.
Cyber liability insurance, indemnification clauses, penalty provisions for SLA failures, and clarity on OCR penalty responsibility ensure financial accountability. Annual audits, vulnerability disclosure reviews, regulatory update notifications, and cybersecurity compliance as renewal criteria maintain ongoing compliance.
CASE STUDIES: REAL-WORLD IMPACT
The Ascension Health ransomware attack (May 2024) disrupted laboratory systems across multiple states, suspending diagnostic testing. The June 2025 MongoDB misconfiguration exposed 8 million patient records. The February 2024 Change Healthcare attack—while not device-specific—disrupted laboratory billing nationwide, demonstrating cascading breach risks in integrated systems.
FUTURE-PROOFING: EMERGING THREATS
AI-driven threats include model poisoning manipulating diagnostic algorithms, inference attacks reverse-engineering proprietary algorithms, and data poisoning corrupting training data. Regulatory evolution through 2026 will bring FDA AI guidance updates, HIPAA Privacy Rule expansion, and EU/global harmonization.
Technology trends include Zero Trust Architecture adoption, Hardware Security Modules for encrypted key storage, blockchain-based audit logs, and quantum-ready encryption. Healthcare organizations must invest in specialized security skills, conduct incident response drills, maintain backup diagnostic capacity, and consider vendor consolidation.
CONCLUSION: BUILDING TRUST IN CONNECTED DIAGNOSTICS
Cybersecurity is no longer optional—regulatory mandates make security table-stakes for market access. The procurement decision is fundamentally a security decision. Evaluate vendors against clear criteria: ISO 81001-5-1 compliance, documented threat modeling, and explicit security SLAs distinguish secure vendors from vulnerable ones.
Integration security is critical, as LIS/HIS integration creates the largest attack surface. Assume breaches will occur; focus on detection speed and data integrity verification. Data privacy directly protects patient safety—unlike other industries, compromised diagnostic analyzers threaten patient outcomes through false results.
For procurement teams: embed ISO 81001-5-1 and FDA cybersecurity standards in RFP requirements. For IT directors: segment connected analyzers on isolated networks; implement continuous monitoring. For compliance officers: include cybersecurity in BAAs; establish penetration testing schedules. For C-suite: recognize that cybersecurity investment protects patient safety and regulatory reputation.
The connected compact hematology analyzer represents the future of diagnostics—rapid, accessible, intelligent. Only when security is embedded from design through deployment can these devices realize their full potential without exposing patients and organizations to unacceptable risk.
Learn more about secure medical device solutions: https://ozellemed.com/en/
Sources Referenced
| Theme | Official Case Links |
| HIPAA Security Rule | https://www.hhs.gov/hipaa/for-professionals/security/index.html |
| FDA Cybersecurity Guidance | https://www.fda.gov/medical-devices/digital-health-center-excellence/medical-device-cybersecurity |
| IVDR (EU) | https://eur-lex.europa.eu/eli/reg/2017/746/oj |
| EU Cyber Resilience Act | https://commission.europa.eu/plug-and-play-digital/secure/cyber-resilience-act_en |
| NIS2 Directive | https://eur-lex.europa.eu/eli/dir/2022/2555/oj |
| HL7 Standards | https://www.hl7.org/implement/standards/ |
| ISO 81001 Series | https://www.iso.org/standard/73040.html |
| NIST TLS Guidance | https://www.nist.gov/publications/digital-identity-guidelines |