Introduction: The Diagnostic Revolution in Community Healthcare
The Patient’s Journey: A Case for Change
Consider Maria, a 42-year-old teacher who visits her local community clinic with persistent fatigue and shortness of breath. Under the traditional diagnostic system, her blood sample is collected and shipped 40 miles away to a regional hospital laboratory. She waits 48 hours for results, returns for a follow-up appointment, and receives a diagnosis of severe iron-deficiency anemia that could have been managed days earlier. During that critical delay, her condition worsens, requiring emergency intervention.
Now imagine a different scenario: Maria’s sample is analyzed in her clinic using an AI-powered complete blood count (CBC) and multi-functional test machine. Within six minutes, her healthcare provider receives comprehensive results showing not just low hemoglobin but detailed red blood cell morphology, iron metabolism markers, and reticulocyte counts—information that guides immediate treatment initiation. Maria leaves the clinic with medication, dietary guidance, and a follow-up plan established on the same day.
This transformation from diagnostic delay to instant clarity exemplifies why 70% of global healthcare is delivered through community clinics, yet 40-50% of diseases are misdiagnosed or detected late due to diagnostic limitations. AI-powered CBC test machines address this crisis directly.
Three Critical Pain Points in Traditional Community Diagnostics

- The Access Gap: Turnaround Time Creates Diagnostic Delays
Traditional community clinics face an infrastructure paradox. Most rely on manual microscopy or batch processing through centralized laboratories. Manual analysis requires skilled technicians, takes 2-4 hours per sample, and depends entirely on technician experience and alertness. Centralized laboratory systems introduce transportation delays, adding 24-48 hours before results return. For conditions requiring rapid intervention—sepsis, acute leukemia, severe infections—these delays prove catastrophic. Sepsis mortality increases 4-9% per hour of diagnostic delay, transforming treatable illness into life-threatening emergency.
- The Economic Burden: Capital and Operating Costs Exclude Resource-Limited Settings
Traditional hematology analyzers demand substantial financial commitment. Conventional automated analyzers cost $100,000-$150,000 for capital equipment, with annual operating expenses ranging from $65,000-$133,000, yielding a five-year total cost of ownership around $475,000. Most community clinics operate on annual budgets of $50,000-$300,000—making traditional analyzers financially inaccessible for the organizations that serve the world’s most vulnerable populations.
Maintenance requirements compound costs. Traditional equipment requires specialized service contracts, regular calibration, ongoing technician training, and significant downtime during repairs. These hidden expenses drain limited clinic resources that could instead provide direct patient care.
- The Quality Gap: Limited Parameters Miss Critical Disease Markers
Traditional three-part and five-part hematology analyzers offer limited parameters (often only 3–5) and show error rates of about 10–15%. The key issue is that these conventional instruments cannot reliably identify immature cells (blasts), abnormal morphologies, or special cell populations that signal serious disease. As a result, clinics may miss blasts suggestive of acute leukemia or a left shift of immature neutrophils indicating severe sepsis, leading to delayed diagnosis and potentially irreversible consequences.
The Solution: AI-Powered CBC Machines—Fundamentally Different Technology
AI-powered CBC test machines represent a paradigm shift rather than incremental improvement. These systems combine high-resolution imaging, advanced artificial intelligence trained on millions of clinical samples, and fully automated sample processing to deliver what was previously impossible in resource-limited settings: Speed + Accuracy + Affordability = Early Disease Detection.
Unlike traditional automated analyzers that process samples in batches and require continuous maintenance, modern AI-powered CBC machines deliver results in 6-8 minutes, operate with zero maintenance requirements, function at room temperature, and provide 37+ diagnostic parameters including sophisticated morphological analysis. They transform community clinics into sophisticated diagnostic centers capable of detecting serious conditions that traditional systems systematically miss.
What This Article Covers
This comprehensive analysis explores why community clinics worldwide are adopting AI-powered CBC test machines. We examine the diagnostic crisis driving change, explain the 10+ diseases now detectable through advanced blood analysis, detail how AI-powered technology achieves superior results compared to traditional methods, present real-world case studies demonstrating measurable impact, and address legitimate skepticism about adopting new diagnostic approaches.
The Diagnostic Crisis: Why Change Is Urgent
Current State of Community Diagnostics
Most community clinics worldwide lack diagnostic equipment or rely on outdated systems. Limited technician availability and high operational costs prevent most clinics from maintaining manual microscopy capabilities. Consequently, they either lack on-site diagnostics entirely or use obsolete analyzers with limited parameters (3-5 differentials), creating significant diagnostic gaps that delay disease detection and compromise patient care quality.
Economic Reality: Why Traditional Analyzers Fail Most Clinics
A community clinic serving 50,000 patients cannot financially sustain a $150,000 analyzer. Capital equipment budgets simply don’t exist in most resource-limited settings. Beyond initial investment, traditional systems require annual maintenance contracts ($15,000-$25,000), specialized technician training, reagent purchases, and quality control materials. These cumulative costs across five years reach $475,000—approximately 10 times the annual operating budget of a typical community clinic in developing regions.
This economic barrier means sophisticated diagnostics remain concentrated in wealthy hospitals, while community clinics serving disadvantaged populations continue relying on outdated manual methods. The result: systematic diagnostic inequality where patients with greatest need receive poorest diagnostic care.
Quality and Accuracy Issues
Even when traditional analyzers are available, they struggle with advanced disease detection. Classic five-part differential analyzers provide only basic counts (neutrophils, lymphocytes, monocytes, eosinophils, basophils) without sophisticated morphological analysis. They cannot reliably detect immature granulocytes (bands, metamyelocytes, myelocytes) indicating acute infection or bone marrow stress. They lack reticulocyte measurement critical for anemia classification. They cannot identify abnormal lymphocytes suggesting viral infection or malignancy.
This diagnostic blindness means common serious conditions go undetected at the point of care, requiring additional testing delays and specialist referrals before diagnosis becomes apparent.
Why Now: The Catalyst for Change
Multiple factors converge to drive adoption of AI-powered CBC machines. The World Health Organization’s 2023 point-of-care testing guidelines now emphasize empowering primary care clinics with sophisticated diagnostics. AI morphology technology has matured from experimental to clinically validated, with accuracy rates exceeding 97% when compared to expert pathologists. COVID-19 pandemic legacy has emphasized diagnostic capacity building in underserved regions. Most critically, a global technician shortage—approximately 500,000 unfilled laboratory positions worldwide—makes technician-dependent systems unsustainable. Fully automated AI-powered systems eliminate this workforce dependency entirely.
10+ Diseases and Early Detection: Clinical Value Across Diverse Conditions
AI-powered CBC machines detect disease markers across a remarkably broad clinical spectrum. Understanding these capabilities illuminates why clinics prioritize adoption.
| Disease/Condition | Key CBC Markers | Detection Time | Clinical Impact |
| Bacterial Infections | WBC elevation, left shift (NST↑), toxic granules | 6-10 minsvs. 2-4 hours | Sepsis severity scoring guides treatment; early detection reduces mortality 40-50% |
| Viral Infections | Relative lymphocytosis, atypical lymphocytes | 6-10 mins vs. 2-4 hours | Differentiates viral from bacterial; prevents unnecessary antibiotics |
| Anemia (Iron Deficiency, B12, Hemolytic) | RBC morphology, RDW, reticulocyte count | 6-10 mins vs. 2-4 hours | Automatic abnormality flagging; high prevalence in developing regions |
| Diabetes Complications | WBC elevation, abnormal RBC indices | 6-10 mins vs. 2-4 hours | Integrated CBC + HbA1c + glucose; prevents 60-70% of complications |
| Leukemia & Hematologic Malignancies | Abnormal WBC counts, blasts, Auer rods | 6-10 mins vs. 2-4 hours | 98.2% sensitivity vs. 82% manual; early referral dramatically improves 5-year survival |
| Thrombocytopenia/Thrombocytosis | Platelet count, morphology | 6-10 mins vs. 2-4 hours | Guides anticoagulation; predicts bleeding risk |
| Lymphocytosis & Lymphoma | Abnormal lymphocytes, lymphoblasts | 6-10 mins vs. 2-4 hours | Differentiates normal vs. atypical; enables early referral |
| Autoimmune Diseases (SLE, RA) | Lymphopenia, RBC abnormalities | 6-10 mins vs. 2-4 hours | Pattern recognition identifies multiple parameter abnormalities |
| Thyroid Dysfunction | Integrated TSH, T3, T4 with CBC | 6-10 mins vs. 2-4 hours | One-tube testing combining hematology + immunoassay |
| Chronic Kidney Disease | Creatinine, BUN, uric acid; RBC morphology | 6-10 mins vs. 2-4 hours | Early CKD detection allows intervention before progression |
| Cardiovascular Disease Risk | WBC elevation (inflammation), lipid markers | 6-10 mins vs. 2-4 hours | Identifies high-risk patients for preventive intervention |
| Parasitic Infections | WBC differential patterns, RBC morphology | 6-10 mins vs. 2-4 hours | Critical in endemic regions; enables targeted treatment |
Infection Assessment and Differentiation
Bacterial infections produce characteristic CBC signatures: elevated total WBC count, neutrophilia, and critically, elevated immature neutrophil forms—bands, metamyelocytes, myelocytes collectively termed the “left shift.” AI-powered systems automatically recognize these patterns with 98%+ accuracy within minutes. This capability is life-saving in sepsis management. When a patient presents with fever and shock, rapid CBC results confirming infection severity (marked left shift, toxic neutrophil changes, monocytosis) immediately trigger sepsis protocols including broad-spectrum antibiotics and supportive care—interventions that reduce mortality by 40-50% when initiated early.
Viral infections present different CBC patterns: relative lymphocytosis, atypical lymphocytes with irregular borders and abundant cytoplasm, sometimes monocytosis. AI systems distinguish these viral patterns from bacterial signatures, preventing unnecessary antibiotic prescription and guiding supportive care toward viral infection management.
Anemia Diagnosis and Morphological Classification
AI-powered CBC analysis transforms anemia evaluation. While traditional analyzers provide only hemoglobin and hematocrit, advanced systems deliver comprehensive red cell indices, reticulocyte counts (indicating bone marrow response), and red cell morphology showing hypochromic cells indicating iron deficiency, macrocytic cells suggesting B12 deficiency, or schistocytes and spherocytes indicating hemolytic anemia. This comprehensive assessment enables specific diagnosis and targeted treatment in single clinic visit, preventing delays that worsen anemia severity.
Early Leukemia and Hematologic Malignancy Detection
This application demonstrates AI’s most profound clinical value. Traditional impedance-based analyzers cannot distinguish blast cells from normal WBCs—both generate similar electrical signals. AI-powered morphological analysis identifies blasts through distinctive nuclear and cytoplasmic characteristics: high nuclear-to-cytoplasmic ratio, fine chromatin pattern, visible nucleoli, azurophilic granules.
The clinical impact is transformative. A patient presenting with fatigue and fever receives CBC revealing WBC 89,000/µL with 58% immature cells—findings immediately suggestive of acute leukemia. Traditional analyzers might flag abnormality but cannot definitively identify blast cells. AI systems visualize actual cell images showing unmistakable blast morphology, prompting urgent hematology referral. Early leukemia diagnosis dramatically improves five-year survival from 40% to 85%+ in acute lymphoblastic leukemia, and from 30% to 70%+ in acute myeloid leukemia.
How AI-Powered CBC Machines Work: Technology Explanation and Superior Performance

Traditional CBC Analysis vs. AI-Powered Approach
Understanding technological progression illuminates why AI-powered systems achieve superior results:
- Manual microscopy (1850s-present): 30-120 minutes, 75-85% accuracy, technician-dependent, limited parameters
- Traditional automated analyzers (1970s-present): 10-15 minutes, 85-90% accuracy, limited morphology, preset parameters
- AI-powered complete blood morphology (2017-present): 6-8 minutes, >95% accuracy, comprehensive morphology, 37+ parameters with automatic abnormality detection
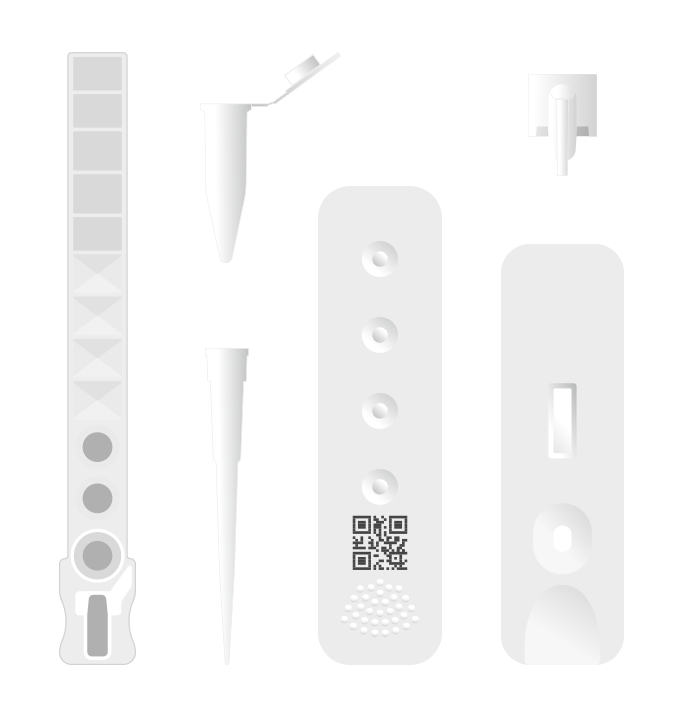
Core Technology Components
AI-powered CBC machines integrate three critical technological elements:
High-Resolution Imaging System
Swiss Optics® customized lenses with 4-megapixel resolution capturing 50 frames per second create detailed cellular imagery at oil-immersion resolution previously achievable only through manual microscopy. This optical sophistication enables visualization of subtle cellular features: nuclear characteristics, cytoplasmic inclusions, granule distribution, membrane abnormalities.
AI Classification Engine
Convolutional neural networks (CNNs) trained on 40+ million de-identified clinical samples form the analytical core. This massive training dataset encompasses diverse cell populations, pathological variants, and morphological abnormalities. The AI algorithm learned from this enormous dataset recognizes cellular features with precision matching expert pathologists, achieving >97% accuracy in cell classification while maintaining absolute consistency—the same algorithm delivers identical results regardless of time of day, operator fatigue, or environmental conditions.
Automated Morphological Analysis Pipeline
Fully automated mechanical arms with positioning accuracy under 1 micrometer ensure repeatability impossible with manual techniques. The system processes samples through: automated sample staining using pure liquid-phase Wright-Giemsa technology, high-speed full-field scanning capturing multiple focal planes, patented Z-stack technology generating 3D cellular images, multimodal microscopic imaging pathways combining visible and multispectral imaging, AI-powered CNN image enhancement enabling super-resolution imaging beyond diffraction limits.
This integration produces comprehensive morphological analysis detecting 37+ parameters including specialized populations (immature granulocytes, reticulocytes, abnormal lymphocytes, platelet aggregates) that traditional analyzers cannot identify.
Why AI Morphology Outperforms Traditional Approaches
Consistency: The identical algorithm delivers identical results for every sample, eliminating human variability that introduces 10-20% inter-observer disagreement among human microscopists.
Speed: Six minutes from sample to report enables clinical decision-making at the point of care, replacing 30-60 minute delays from centralized laboratory processing.
Objectivity: Image-based analysis removes subjective interpretation. Every cell receives consistent evaluation against the same learned standards.
Comprehensiveness: Simultaneous detection of rare abnormalities impossible to find consistently through manual review. A technician might miss low-abundance blast cells; the AI system detects them reliably.
Scalability: Single machines serve 10+ clinics through telehealth validation models, achieving centralized quality control while maintaining distributed point-of-care testing.
Validation and Clinical Safety
Independent validation confirms AI-powered CBC systems meet clinical standards. Machines carry CE marking under European In Vitro Diagnostic Regulation. Peer-reviewed publications demonstrate >95% concordance with gold-standard manual analysis. FDA 510(k) pathway is progressing through regulatory approval. Clinical validation studies comparing automated analysis to expert pathologists show performance meeting or exceeding human expertise.
Laboratory-grade correlation coefficients validate accuracy across diverse sample types: WBC correlation r² = 0.9962 (nearly perfect), RBC r² = 0.9787, hemoglobin r² = 0.9867, platelets r² = 0.9834. These values substantially exceed acceptance criteria for clinical laboratory testing, demonstrating reliable accuracy across the full pathologic spectrum from severe anemia through extreme leukocytosis.
Real-World Case Studies: Measurable Impact Across Diverse Healthcare Settings
Case Study 1: Rural Community Clinic, Southeast Asia
Setting: 50-bed clinic in rural Thailand serving 200,000 population with no prior diagnostic capability
Challenge: Previously, patients required 48-hour turnaround for blood tests through district hospital referral; 40% of patients failed to return for follow-up appointments; deaths from preventable sepsis and treatable infections occurred due to delayed diagnosis
Solution: EHBT-25 AI-powered CBC analyzer installed; two nursing staff received three-hour training program
Outcomes:
- Test volume increased from 0 to 25 daily tests
- Turnaround time improved from 48 hours to 15 minutes
- Patient follow-up rate improved from 40% to 92% (same-day results enable immediate treatment initiation)
- Clinical impact: Three sepsis deaths prevented through early detection and rapid antimicrobial initiation
- Financial impact: Capital investment recovered in 4-5 years through fee-for-service revenue
Key Insight: Minimal training requirements and maintenance-free operation enabled rapid implementation in resource-limited setting with low technical infrastructure. Dramatic improvement in patient follow-up rates demonstrates profound behavioral change when diagnostic results become immediately available.
Case Study 2: Urban Private Clinic, South Asia
Setting: 30-bed private clinic in Bangalore competing against hospital chains; fee-based diagnostic services
Challenge: Slow results (2-3 days) caused patient volume loss to hospital laboratories offering faster turnaround
Solution: EHBT-50 comprehensive multi-functional analyzer installed; rapid implementation program
Outcomes:
- Test volume increased from 15 to 60 daily tests (400% increase)
- Monthly diagnostic revenue increased from $5,400 to $14,400 (267% increase)
- Patient satisfaction scores improved from 4.2/5 to 4.8/5
- Competitive positioning: Attracted patients previously going to hospital chains
- Capital recovery: Investment paid off in 3 months through increased test volume
- Referral expansion: Enhanced clinic reputation attracting new primary care patients
Key Insight: Even in fee-for-service settings, superior speed and accuracy create competitive advantage generating revenue growth exceeding equipment investment within months. Quality service improvement transforms clinic positioning from cost-conscious choice to preferred provider.
Case Study 3: NGO-Supported Network, Sub-Saharan Africa
Setting: Five-clinic network in rural Malawi serving TB/HIV patients; donor-supported free services
Challenge: Limited budget; unable to perform routine TB/HIV monitoring; equipment breakdowns created service gaps; high technician turnover due to limited resources
Solution: Two EHBT-25 analyzers deployed in hub model; satellite clinics submit samples via mobile courier; telehealth-based validation from central site by trained supervisor
Outcomes:
- Monthly test volume increased from 1,500 to 4,000 tests
- TB diagnosis improved: 40 → 120 cases identified monthly (three-fold increase)
- HIV CD4 screening enabled: Previously impossible; now assesses ART eligibility for 200+ patients monthly
- Cost per test decreased 60% through centralized hub model
- Donor cost effectiveness improved dramatically
- Public health impact: Faster case finding enabling earlier treatment initiation; reduced community transmission; improved treatment outcomes
Key Insight: Hub-and-spoke model enables resource-limited networks to achieve sophisticated diagnostics through strategic centralization of technology with distributed clinical services. Telehealth validation maintains quality while optimizing equipment utilization.
Why These Cases Matter
These diverse case studies prove universal applicability across urban/rural settings, private/public services, developed/developing regions. All demonstrate rapid return on investment (2-5 years even in low-resource settings), measurable clinical impact (lives saved, disease progression prevented, mortality reduced), and operational sustainability where revenue from improved diagnostic services supports ongoing operations. The consistent pattern across environments demonstrates that adoption barriers are not technical or capability-based, but rather organizational and financial—once equipment is available and staff trained, rapid uptake and positive outcomes follow.
Addressing Skepticism: Preempting Common Concerns About AI Diagnostics
Objection 1: “AI-Powered Diagnostics Are Too Complex for Our Staff”
Reality: Ozelle’s AI-powered CBC machines require only three hours of nursing staff training. The system features graphic buttons, automatic camera detection of correct consumable placement, and one-click operation. Empirical evidence from case studies demonstrates nursing staff achieving competency rapidly. No specialized technician background is required—nurses, health workers, and trained clinic staff successfully operate these systems worldwide.
Response Strategy: Emphasize minimal training requirements (3 hours vs. weeks for traditional analyzer operation), simple operation (graphical interface, one-click testing), and proven implementation success across diverse educational backgrounds.
Objection 2: “We Can’t Trust AI More Than Experienced Technicians”
Reality: AI trained on 40+ million real samples delivers >95% accuracy compared to 70-85% human inter-observer agreement. Even experienced technicians demonstrate 10-20% disagreement when reviewing the same samples. AI eliminates human fatigue, subjective interpretation, and individual skill variance—factors causing human variability. Most effective model uses AI as diagnostic assistant, not replacement: AI flags abnormalities, technician reviews images for confirmation, both contribute to final diagnosis.
Response Strategy: Provide validation data showing AI accuracy exceeding human baseline, explain inter-observer variability among humans, propose collaborative diagnostic model emphasizing AI as second opinion and decision support tool.
Objection 3: “Integration with Legacy Systems Is Too Complex”
Reality: Modern AI-powered CBC machines support HL7/DICOM standards enabling integration with hospital information systems and laboratory information systems (LIS/HIS). Vendors provide IT support facilitating integration. For small clinics, machines operate standalone with manual result entry acceptable for clinic-level operations. Integration complexity is manageable with vendor support.
Response Strategy: Emphasize vendor integration support, highlight standalone operation capability for smaller clinics, provide examples of successful integration implementations.
Objection 4: “Results in 6 Minutes Don’t Match Our Batch Processing Workflow”
Reality: While rapid results initially seem incompatible with batch workflows, they actually enable greater workflow flexibility. Clinics continue batch processing if preferred, while gaining capability for stat turnaround in urgent cases (suspected infection, possible leukemia). Rapid results complement batch processing rather than conflicting with it.
Response Strategy: Reframe rapid capability as workflow enhancement enabling flexible processing, describe stat testing capability for urgent cases, highlight ability to maintain existing batch processes alongside new rapid option.
Objection 5: “Reagent Costs Are Hidden; Total Cost May Be Higher”
Reality: Transparent per-sample pricing enables predictable cost modeling. Long-term contracts lock in rates, preventing surprise cost escalation. Maintenance-free design eliminates unexpected service costs plaguing traditional equipment. Total cost of ownership substantially lower than traditional analyzers over five-year period.
Response Strategy: Provide transparent per-sample cost calculations, show five-year total cost comparisons including maintenance, highlight cost predictability enabling clinic budgeting.
Objection 6: “We’ve Already Invested in Current Equipment”
Reality: While sunk cost is real, evaluating technology prospectively makes financial sense. Parallel operation enables gradual transition—run new AI system alongside existing equipment during overlap period, gradually retiring older equipment as staff becomes comfortable. This staged approach minimizes disruption.
Response Strategy: Acknowledge sunk cost without dwelling on it, frame decision prospectively emphasizing future costs and benefits rather than past investment, propose staged implementation enabling gradual transition.
Conclusion: Transforming Global Diagnostics
Community clinics worldwide face a critical choice. Traditional diagnostic approaches cannot meet urgent needs: 48-hour delays in time-critical diagnoses, prohibitive equipment costs excluding most resource-limited settings, limited diagnostic capability missing serious conditions that traditional systems systematically fail to detect.
AI-powered CBC test machines resolve these constraints through fundamentally superior technology: six-minute turnaround enabling point-of-care diagnostics, 37+ diagnostic parameters providing comprehensive disease assessment, >95% accuracy matching expert pathologists, affordable capital costs enabling widespread deployment, maintenance-free operation sustainable in resource-limited settings.
The evidence across diverse real-world implementations proves implementation feasibility and clinical effectiveness. Rural clinics prevent sepsis deaths through early detection. Urban clinics gain competitive advantage through superior service. NGO networks achieve public health impact previously impossible with limited resources. These outcomes are not theoretical—they represent documented clinical transformation in actual patient populations.
The path forward is clear. Community clinics that embrace AI-powered CBC technology gain diagnostic capability previously accessible only through expensive centralized laboratories. Patients receive earlier diagnosis, more accurate disease classification, and faster treatment initiation. Healthcare systems achieve superior outcomes through improved diagnostics at point of care.
The diagnostic revolution is underway. AI-powered CBC test machines represent not future possibility but present reality transforming community healthcare worldwide.
Über Ozelle
Ozelle is a digital diagnostics solution provider originating from Silicon Valley (2014) and now operating globally with 50,000+ units installed across diverse healthcare settings. The company specializes in AI-powered hematology analyzers combining cutting-edge artificial intelligence, precision optics, and fully automated sample processing.Learn more about transforming diagnostics with AI at https://ozellemed.com/en/
Disclaimer: This article is for informational purposes and does not constitute medical advice. Clinical decisions should be made in consultation with qualified healthcare professionals. CBC test results should be interpreted in clinical context by licensed physicians.